Endocrine
Thyroid Disorders
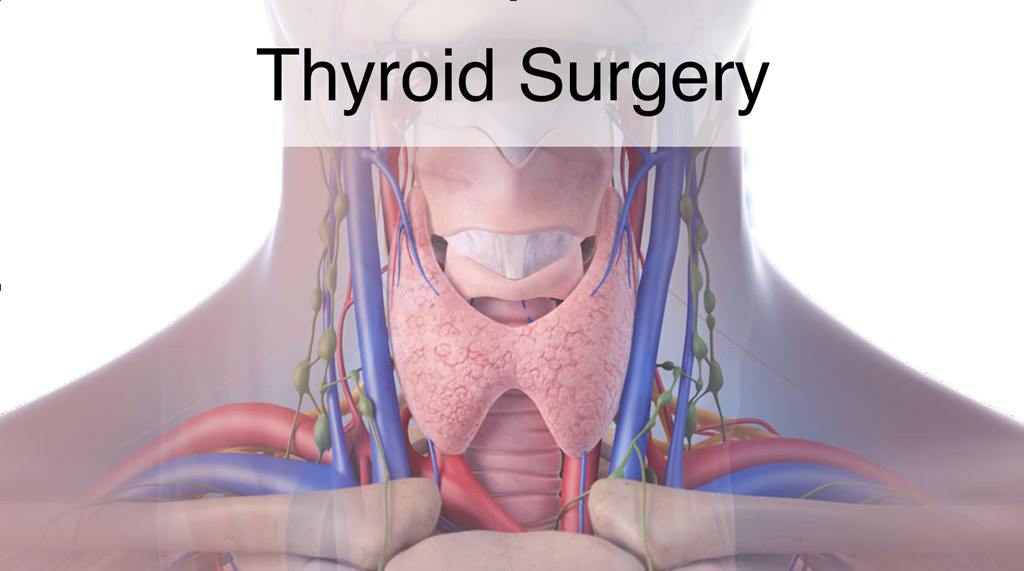
Thyroidectomy is the removal of all or part of your thyroid gland. Your thyroid is a butterfly-shaped gland located at the base of your neck. It produces hormones that regulate every aspect of your metabolism, from your heart rate to how quickly you burn calories.
Thyroidectomy is used to treat thyroid disorders, such as cancer, noncancerous enlargement of the thyroid (goiter) and overactive thyroid (hyperthyroidism).
The extent that the thyroid gland is removed during thyroidectomy depends on the reason for surgery. If only a portion of the gland is removed (partial thyroidectomy), your thyroid may be able to function normally after surgery. If your entire thyroid is removed (total thyroidectomy), you need daily treatment with thyroid hormone to replace your thyroid’s natural function.
Indications
A thyroidectomy may be recommended for conditions such as:
- Thyroid cancer. Cancer is one of the most common reasons for thyroidectomy. If you have thyroid cancer, removing most, if not all, of your thyroid will likely be a treatment option.
- Noncancerous enlargement of the thyroid (goiter). Removing all or part of your thyroid gland is an option if you have a large goiter that is uncomfortable or causes difficulty breathing or swallowing or, in some cases, if the goiter is causing hyperthyroidism.
- Overactive thyroid (hyperthyroidism). Hyperthyroidism is a condition in which your thyroid gland produces too much of the hormone thyroxine. If you have problems with anti-thyroid drugs and don’t want radioactive iodine therapy, thyroidectomy may be an option.
Risks
Thyroidectomy is a safe procedure, and the complication rate is very low.
Potential complications include:
- Bleeding
- Infection
- Airway obstruction
- Permanent hoarse or weak voice due to nerve damage
- Damage to the four small glands located behind your thyroid (parathyroid glands), which can lead to abnormally low calcium levels and an increased amount of phosphorus in your blood
Preparing for Surgery
If you have hyperthyroidism, your doctor may prescribe medication — such as an iodine and potassium solution — to regulate your thyroid function and decrease the risk of bleeding.
You will need to avoid eating and drinking after midnight the night before surgery, as well, to avoid anesthesia complications.
What you can expect
Your surgery will be performed under general anesthesia, so you won’t be conscious during the procedure. The anesthesiologist or anesthetist gives you medication to make you sleep during the procedure. A breathing tube will then be placed in your trachea to assist breathing throughout the procedure.
The surgical team places several monitors on your body to help make sure that your heart rate, blood pressure and blood oxygen remain at safe levels throughout the procedure. These monitors include a blood pressure cuff on your arm and heart-monitor leads attached to your chest.
Once you’re unconscious, the surgeon makes a small incision in the center of your neck or a series of incisions some distance from the thyroid, depending on the surgical technique used. All or part of the thyroid gland is then removed, depending on the reason for the surgery.
If you’re having thyroidectomy as a result of thyroid cancer, the surgeon may also examine and remove lymph nodes around your thyroid. Thyroidectomy usually takes a few hours.
After surgery, you’re moved to a recovery room where the health care team monitors your recovery from the surgery and anesthesia. Once you’re fully conscious, you’ll be moved to a hospital room.
You may have a drain under the incision in your neck. This drain is usually removed the morning after surgery.
After a thyroidectomy, you may experience neck pain and a hoarse or weak voice. This hoarseness doesn’t necessarily mean there’s permanent damage to the nerve that controls your vocal cords. These symptoms are often temporary and may be due to irritation from the breathing tube (endotracheal tube) that’s inserted into your windpipe (trachea) during surgery or as a result of nerve irritation caused by the surgery.
You’ll be able to eat and drink as usual after surgery. You will stay overnight in the hospital.
When you go home, you can usually return to your regular activities. Wait until you are off of pain medications before driving.
Results
The long-term effects of thyroidectomy depend on how much of the thyroid is removed.
Partial thyroidectomy
If only part of your thyroid is removed, the remaining portion typically takes over the function of the entire thyroid gland, and you likely will not need thyroid hormone therapy.
Complete thyroidectomy
If your entire thyroid is removed, your body can’t make thyroid hormone and without replacement you’ll develop signs and symptoms of underactive thyroid (hypothyroidism). As a result, you’ll need to take a pill every day that contains the synthetic thyroid hormone levothyroxine (Levoxyl, Synthroid, Unithroid).
This hormone replacement is identical to the hormone normally made by your thyroid gland and performs all of the same functions. Your doctor will determine the amount of thyroid hormone replacement you need based on blood tests.”
Parathyroid Disorders

What are the parathyroids?
The parathyroids are four tiny glands in your neck, two on each side of your thyroid gland. They make parathyroid hormone (PTH) which controls the level of calcium in the blood. Calcium is very important for the normal functioning of muscles, nerves, and bones. It is absorbed through the intestines and stored in the bones. Parathyroid hormone raises blood levels of calcium by increasing intestinal absorption of calcium, and by dissolving calcium from the bone into the bloodstream.
What is hyperparathyroidism?
Some people make too much parathyroid hormone, a condition called hyperparathyroidism. This condition is most common in middle-aged women, but can occur in men or women at any age and can run in families. In 9 of 10 patients with hyperparathyroidism, the cause is a single benign tumor. In one of 10, all four parathyroids are enlarged. Cancer is exceedingly rare.
What are the symptoms of hyperparathyroidism?
The body does not like having blood calcium levels too high, and tells you in a number of ways.
Hyperparathyroidism can cause
- Weak bones, called osteoporosis, which can lead to fractures
- Kidney stones, renal impairment
- High blood pressure
- Abdominal pain
- Increased frequency of urination
- Constipation
- Stomach ulcers and pancreatitis
- Psychiatric problems
- Arrythmias and heart disease
- Difficult to control blood sugar if you are diabetic
- Other symptoms are much more subtle and include
- Weakness and fatigue, loss of energy
- Memory and concentration problems
- Muscle and joint aches and pains
- Abdominal and back pains
- Feeling “older” than you should
- Mood swings or depression
IMPORTANT ***These non-specific, vague symptoms happen with high calcium no matter if it’s only slightly high or very high. High calcium is never normal and should not be “watched.” These vague symptoms improve in 85% of patients after successful parathyroid surgery. Most patients who thought they had no symptoms, in retrospect, realize they did have these symptoms and feel much better within weeks after surgery. They frequently say things like: “I feel 10 years younger,” and “you have given me a new body.” Bone density also improves, reducing the risk of fractures.***
Treatment of hyperparathyroidism
The only effective treatment for hyperparathyroidism is surgery to remove the overactive gland(s). In the hands of an experienced endocrine surgeon, surgery can cure the condition in 98% of cases. There is no effective non-surgical treatment for hyperparathyroidism. Before surgery, you will have a sestamibi scan (a painless scanning test) and a neck ultrasound to see if there is one enlarged gland that can be located.
If the abnormal gland is seen, you can have “parathyroid mini-surgery” through a very small incision, and possibly go home the same day. Even if the gland is not seen, it can still be found at surgery in 98% of cases. The surgery takes about one hour, and the incision is on your neck. You will be completely asleep during the operation and will feel no pain. Recovery is quick, with most patients going home the same day or the next day, and feeling very little discomfort. Most are back at work in a few days!
Frequently Asked Questions
Is there any other treatment besides surgery?
No. Surgery is the only effective treatment of hyperparathyroidism.
What if I don’t have the surgery?
Even if you think you have no symptoms, you will almost certainly feel much better after you are cured. If you don’t have surgery, you will continue to have high blood calcium, and many symptoms listed above. Without surgery, your bones will continue to become weaker, and possibly break. There is evidence of increased risk of high blood pressure, stroke, heart disease, and even shorter life expectancy, from untreated hyperparathyroidism.
How long will I be hospitalized?
Most patients are able to go home the same day (after parathyroid “mini-surgery”) or the following day.
What type of anesthesia will I have?
You will have a general anesthesia. You will be completely asleep during the operation.
When will I know the results of the surgery?
The calcium levels generally return to normal within 12-48 hours of surgery.
Will I have a scar?
Yes. All surgery causes scarring, and how a patient scars are dependent on the individual. However, there are some techniques that surgeons use to minimize scarring. These techniques include careful incision placement and hypoallergenic suture material (to avoid inflammation).For parathyroid “mini-surgery,” the scar is about 1-2 inches. If you need a full neck exploration, it will be bigger. As a general rule, no matter which operation you need, it is unusual to have a very noticeable scar after six months. Scars continue to fade for three years.
Will I have pain after the operation?
All operations involve some discomfort, but most patients are surprised at how little pain they feel after this operation. Although you should be able to eat and drink normally, the main complaint is a sore throat and discomfort with swallowing for 1-2 days. Most patients take over the counter pain meds such as ibuprofen or acetaminophen to keep them comfortable at home. You will have a prescription for something stronger for the first few days in case you need it, but beware prescription pain medicine can make you drowsy and constipated, so do not drive, drink lots of water and eat plenty of fruits and vegetables.
Will I have stitches?
You will have stitches on the inside that dissolve on their own. You will have a waterproof Comfeel dressing so that you can shower or bathe as usual (but do not submerge the incision for 5 days). Leave the dressing in place until your first post-operative visit, where it will be removed.
Will I have any physical restrictions after my surgery?
Your activity level depends on the amount of discomfort you experience. Many patients have resumed golf or tennis within a week after the operation. Most patients return to work in a week, and you are able to drive as soon as your head can be turned comfortably without prescription pain pills (this limitation is for driver safety).
What are the possible complications of parathyroid surgery?
The nerves that control your voice are very closely associated with the parathyroid glands. Temporary voice changes are not uncommon but usually resolve within weeks to months. In 1 in 100 parathyroid operations, the nerves that control the voice are permanently affected. When this occurs, the main difficulties are the projection of the voice and production of high pitched sounds. It is usually described as hoarse, but will not necessarily be considered abnormal by strangers.
Sometimes the surgery will not cure the hyperparathyroidism. In the hands of an experienced endocrine surgeon, failure to cure occurs in fewer than 2 in 100 patients. Sometimes the normal parathyroid glands become “lazy” because the abnormal gland was doing all the work. They may take some time to recover, so some patients require extra calcium tablets on a temporary basis. Rarely, the parathyroids do not recover, and calcium and vitamin D may be needed on a permanent basis. In rare instances, the tumor can recur. Lifelong yearly blood tests are recommended.
There is a small risk of bleeding into the wound. If this happens, it may be necessary to have a second operation to evacuate the blood so it does not interfere with your breathing. Infection is relatively uncommon, and is easy to treat should it occur.
WHAT ARE THE RISKS OF PARATHYROID SURGERY?
As with anything in life, there are risks to surgery. These risks are weighed against the risks of not having surgery. Listed below are some of the possible complications of surgery. Risks include, but are not limited to:
- Permanent voice hoarseness…………………………<1%
- Failure to cure the hyperparathyroidism…………..<2%
- Permanent hypoparathyroidism………………………< ½ % (0% for mini-surgery)
- Infection of Incision……………………………………….Less than 1%
- Haematoma or Bleeding…………………………………Less than 1%
- Seroma (fluid collection)…………………………………1% (temporary)
- Swelling and black/blue………………………………….About 5% (temporary)
- Keloid or overgrown scar…………………………………rare
- Other unforeseen risks
You will require general anesthetic, given by a specialist anesthetist. Risk of a serious complication in a healthy person is very rare. Potential risks include, but are not limited to: - Heart problems (death, heart attack, arrhythmias)
- Lung problems (pneumonia, wheezing)
- Blood clots (stroke, clots in leg veins or lungs)
- Drug reactions (also possible with local anesthetic)
- Chipped teeth
- Other unforeseen risks You will meet the anesthetist before your operation and have the chance to discuss these further.
PREPARATION for SURGERY
- Please shower at home the evening before surgery or in the morning
- Please do not shave the surgical site! It will be done for you if necessary. Shaving yourself may increase the risk of infection
- For morning surgery, Do Not Eat or Drink anything after midnight the night before surgery unless otherwise instructed. This includes coffee, tea, water, and juice! Medication with a small sip of water is OK. For afternoon surgery, a small breakfast BEFORE 7 AM is OK, and nothing after that. Your surgery may be canceled if you do not follow these instructions
- Do Not Drink Alcoholic beverages 24 hours prior to your surgery
- Do Not Smoke for 4 weeks before surgery or your risk of serious complications increases
- Ask us if you are permitted to take your routine medications (such as those for heart, blood pressure, or insulin etc.) before arriving for surgery
- Stop aspirin, warfarin, or any other blood thinner 5-7 days prior to surgery
- Do Not bring valuables such as money, jewelry etc. Do not wear make-up
- Bring toiletries and loose fitting, comfortable clothing to wear upon discharge
- You will be required to remove contact lenses, jewelry, dentures, and wigs
- Arrange for a responsible adult to drive you home after discharge
- Notify us if there is a change in your condition prior to surgery (such as a cold, cough, fever or infection). If severe, your surgery may need to be postponed for your safety
- Stop all herbal medications 4 weeks before surgery unless discussed beforehand. Especially Ginseng, Garlic, and Gingko, or St. John’s Wort, which increase the risk of bleeding
THE DAY of YOUR SURGERY
- If you have not already done so, you will meet your anesthetist
- You may need a blood test or ECG prior to surgery
- After the operation, you will some time in the recovery room before going to the ward After discharge, you are not permitted to:
- Drive a Car nor operate power equipment
- Drink Alcoholic Beverages
Post-Operative Instructions for Parathyroid Surgery
Below are general instructions for patients who have had thyroid or parathyroid surgery. Since individual circumstances may vary, it is important that you discuss your individual post-operative care with us.
Monitoring Your Progress
You should feel improvement every day after surgery. If you have any questions regarding your progress, call our office. You should make a follow-up appointment approximately 1-2 weeks after your surgery.
Incision
Your incision is covered with a waterproof protective dressing. You can shower and wash your hair as usual, but do not soak or scrub the dressing. After showering, pat dry. Your dressing will be removed at your first post-operative visit.
If you experience itching once the dressing is off, you may apply lotion to the scar. You might notice bruising around your incision or upper chest and slight swelling behind the scar when you are upright. In addition, the scar may become pink and hard. This hardening will peak at about 3 weeks and may result in some tightness or difficulty swallowing, which will disappear over the next 3 to 4 months. You will also notice some numbness of the skin of your neck. This will gradually improve over time.
Pain
The main complaint following parathyroid surgery is discomfort with swallowing. Some people experience a dull ache, while others feel a sharp pain. This should not keep you from eating anything you want, but the pain can be annoying for a day or two.
You may feel like you have phlegm in your throat. This is usually because there was a tube in your windpipe while you were asleep that caused irritation that you perceive as phlegm. You will notice that if you a cough, very little phlegm will come up. This should clear up in 4 to 5 days.
Voice Changes
Your voice may go through some temporary changes with fluctuations in volume and clarity (hoarseness). Temporary changes are quite common. Generally, it will be better in the mornings and “tire” toward the end of the day. This can last for variable periods of time but should clear in 4-6 months at most. There is a small (1/100) risk of permanent hoarseness.
Hypocalcemia and Bone Health
Your bones have been starved of calcium during the time you have had hyperparathyroidism, and will now have the chance to grow strong again. After successful parathyroid surgery, I recommend you take Caltrate Plus twice a day (available at any chemist) to promote healthy bones. In addition to these supplements, an exercise routine using weights is also recommended.
In about 20% of patients who have parathyroid surgery, the remaining parathyroid glands have become lazy, and do not function properly immediately after surgery. This is usually temporary and causes the blood calcium level to drop below normal (hypocalcemia). Symptoms of hypocalcemia include numbness and tingling in your hands, soles of your feet and around your lips. Some patients experience a “crawling” sensation in the skin, muscle cramps or headaches. These symptoms appear between 24 and 48 hours after surgery. It is rare for them to appear after 72 hours.
Hypocalcemia is treated with extra calcium tablets. You should purchase Calcium with Vitamin D (Caltrate) tablets before surgery so you have them at home. If you feel you need it, take two extra tablets (there is no danger in taking it, even if you do not need it.) The symptoms of tingling/numbness should improve within 30 minutes of taking the tablets. If they do not disappear, you should call my office.
You should repeat the dose whenever the symptoms return. This may mean that you are taking as many as 2 tablets every 3 hours. It is important that you keep us informed. The hypocalcemia should disappear over a few weeks. If it does not, let us know.
CONTACT MY OFFICE for any of the following symptoms:
- Fever >100.5 or chills
- Increasing pain or redness around incision
- Difficulty breathing
- Tingling around the lips or fingertips not relieved by calcium tablets
- Severe muscle cramps
AN IMPORTANT WORD ABOUT THE COSTS OF TREATMENT
Insurance rebates have not kept pace with the cost of running a medical practice. As a consequence, there will be a gap to pay for the surgical fee and for the anesthetist. Your insurance company might also charge you an excess for a hospital admission. We will advise you about expected out-of-pocket costs not covered by insurance. If these costs represent an undue hardship for you, please discuss them with us.
ASK YOUR DOCTOR
We are here to help you. If you have any questions, please ask. It is often helpful to bring a family member with you to a consultation or to write questions down so you won’t forget them.
Adrenal Surgery
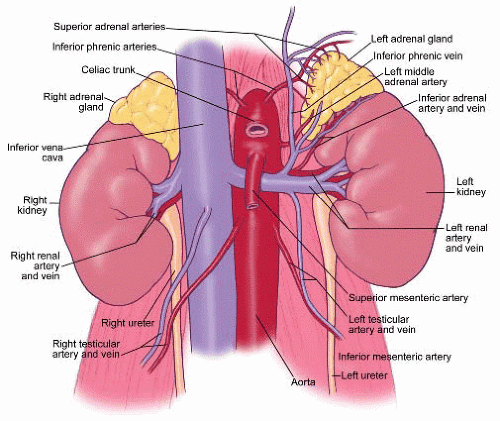 Adrenal surgery has been revolutionized recently with the advent of operative laparoscopy. A laparoscope is like a telescope and through this “minimally invasive” approach an adrenal gland can be removed, thereby minimizing the amount of post-operative pain and the overall recovery period. In some patients with very large tumors of the adrenal gland (>8 cm) or other confounding problems, the laparoscopic approach is not recommended and the standard, larger incision is preferred. However, in most patients requiring an adrenalectomy, the laparoscopic approach is appropriate.
Adrenal surgery has been revolutionized recently with the advent of operative laparoscopy. A laparoscope is like a telescope and through this “minimally invasive” approach an adrenal gland can be removed, thereby minimizing the amount of post-operative pain and the overall recovery period. In some patients with very large tumors of the adrenal gland (>8 cm) or other confounding problems, the laparoscopic approach is not recommended and the standard, larger incision is preferred. However, in most patients requiring an adrenalectomy, the laparoscopic approach is appropriate.
Laparoscopic adrenalectomy is now being performed on a routine basis at our centre. The benefits of the minimally invasive approach are quite clear in regard to postoperative pain and length of hospitalization. Most patients require only a single night hospital stay after the surgery. Patients report a requirement for pain medications that lasts an average of 2-3 days with a “return to normal activities” by 5-7 days. These results represent a significant improvement compared to the standard open adrenalectomy that has been done in the past.

